 |
 |
AbstractBackground and Objectives We analyzed the data of oropharyngeal squamous cell carcinoma (OPSCC) patients who had transoral surgery with/without adjuvant therapy and experienced recurrence. From the data, the treatment outcomes and prognostic factors of recurrent OPSCC were evaluated, and the predictive factors related to successful salvage treatment were identified.
Subjects and Method We used data from patients who were diagnosed with OPSCC and received transoral surgery at the hospital from January 2005 to December 2019.
Results The 5-year survival rate of patients with recurrent OPSCC was 43.9%. The predictors of successful salvage treatment were adjuvant therapy and the p16 status. The 5-year survival rate following salvage treatment for patients who had recurrent OPSCC and also tested p16-positive was 64%; however, it was only 30% for patients who had recurrent OPSCC and tested p16-negative. The 5-year survival rate was 22% for patients who received adjuvant therapy and 64% for those who did not receive it.
Conclusion In OPSCC patients who recurred after transoral surgery with/without adjuvant therapy, the salvage treatment success rate was 45%. In recurrent cancer, the HPV status was an important factor associated with successful salvage treatment, as the success rate of salvage treatment was remarkably high in patients who did not receive adjuvant therapy. Thus, we verified that it is crucial to conduct an initial surgery with clear margins and determine the optimal criteria for adjuvant therapy.
IntroductionRecently, the incidence of oropharyngeal squamous cell carcinoma (OPSCC) caused by smoking and drinking has gradually decreased, and the incidence of human papillomavirus (HPV)-associated OPSCC has continuously increased [1]. Traditionally, many surgical methods have been applied in the treatment of OPSCC, but the high morbidity associated with complex reconstructive surgery or extensive resection has been a problem [2,3]. Concurrent chemoradiation (CCRT) is widely used for OPSCC treatment after previous research of comparable oncological and superior functional outcomes of CCRT compared to conventional surgical treatment [3]. However, CCRT also has high toxicity, and delayed dysphagia may be a problem due to soft tissue fibrosis induced by radiotherapy. Therefore, a new treatment method is needed that can preserve organ function with acceptable oncologic results comparable to existing treatment modalities while having low associated morbidity.
Along with the development of robotic and endoscopic technology, transoral surgery is used in the treatment of OPSCC [4]. Transoral surgery has the advantage of lower morbidity and rapid recovery after surgery compared to conventional surgical methods. In addition, comparable oncological results of transoral surgery for treatment of OPSCC have been reported [5-7]. The advantage of surgical treatment including transoral surgery is that it is possible to assess the risk stratification by exploring pathological factors related to prognosis based on surgical specimens and to administer intensified or de-intensified therapy to appropriate patient groups. If adjuvant radiotherapy is not performed in low-risk patients, the aftereffects of radiotherapy can be avoided, and radiotherapy can be available if the disease recurs later. In addition, since the surgical extent of transoral surgery is relatively small, the possibility of salvage surgery in patients with local recurrence increases. In this study, we analyzed the medical data of OPSCC patients who received transoral surgery with/without adjuvant therapy and experienced recurrence. The treatment outcomes and prognostic factors of recurred OPSCC patients were analyzed and the predictive factors related to successful salvage treatment were identified.
Subjects and MethodsPatients who were diagnosed with OPSCC and received transoral surgery at Severance Hospital from January 2005 to December 2019 were included in the study. The Institutional Review Board of Yonsei University College of Medicine approved this retrospective study (2024-0292-001). Tumor stages of all patients were calculated using the 8th edition American Joint Committee on Cancer staging system. The inclusion criteria were as follows: 1) histologically diagnosed with OPSCC and received transoral surgery with curative intent. Exclusion criteria were 1) previous head or neck surgery or radiation therapy, 2) distant metastasis at the time of surgery, 3) distant metastasis at the time of salvage therapy and 4) follow-up was not conducted for a sufficient period after treatment.
The patientвАЩs age, sex, smoking history, and drinking history were investigated based on medical records. The patientвАЩs age was based on their age at the time of the initial diagnosis. Former smokers and current smokers were considered as smoking patients and so as alcohol drinker. Tumor stages of all patients were investigatied based on pathological staging. Pathological information including surgical margin status, lymphovascular invasion (LVI), perineural invasion (PNI), extranodal extension (ENE), and tumor size were investigated. The presence or absence of disease recurrence was investigated and classified into local and regional according to the site of recurrence. The time from the initial treatment to the detection of disease relapse was defined as the recurrence period. During the study period, the death of the patient and the cause of death were investigated. Based on the recurrence and death data, survival of recurrent OPSCC patients was analyzed.
All patients included in this study received transoral surgery with/without adjuvant therapy as the initial treatment with curative intent. Elective neck dissection was administered for N0, and modified radical neck dissection was administered for N+. Adjuvant therapy (radiotherapy or CCRT) was considered for a positive/close margin; for LVI, PNI, or ENE; for T3-4 findings in postoperative pathological examination results. The salvage treatment method for recurred patients was determined by explaining the pros and cons of each treatment modality and by interviewing the patient.
Multivariate analyses were conducted to identify the prognostic factors influencing patient survival. Chi-square or FisherвАЩs exact test was used to evaluate differences in categorical variables between two independent groups. An independent two-sample t-test was used to assess differences in continuous variables between two independent groups. The multivariate Cox proportional hazards regression model was used to simultaneously evaluate the effects of several factors on patient survival. The Kaplan-Meier curve was used to analyze disease-specific survival, and the survival outcomes were assessed using a log-rank test. A p-value <0.05 was considered to indicate statistical significance. Statistical analyses were performed using IBM SPSS Statistics software Version 18.0 (SPSS Inc., Chicago, IL, USA).
ResultsA total of 57 recurrent OPSCC patients was included in this study. There were 51 males (89.5%) and 6 females (10.5%). The mean age of the patients was 60.8 years (range, 42-81). The tumor T classification at the time of initial surgery was T1 in 23 patients (40.4%), T2 in 26 patients (45.6%), T3 in 6 patients (10.5%), and T4 in 2 patients (3.5%). The N classification was N0 for 15 patients (26.3%), N1 for 18 patients (31.6%), N2 for 15 patients (26.3%), and N3 for 9 patients (15.8%). In 57 patients whose disease recurred, the stage of the recurred tumor was recalculated as T0 in 34 patients, T1 in 11 patients, T2 in 5 patients, T3 in 2 patients, and T4 in 5 patients. In the N classification, N0 was 19, N1 was 26, N2 was 10, and N3 was 2.
After transoral surgery, 38 cases (66.7%) showed negative margins, and 19 cases (33.3%) showed positive margins. LVI was found in 19 cases (33.3%), and PNI was found in 7 cases (12.3%). ENE was present in 25 cases (43.9%). Adjuvant therapy was performed in 26 patients (45.6%), radiotherapy alone in 7 patients, and CCRT in the remaining 19 patients. Among the 57 patients with recurrence, there were 18 cases of local recurrence, 33 cases of regional recurrence and 6 cases of loco-regional recurrence. A total of 26 patients eventually died due to recurrent disease. Table 1 summarizes the clinical information of patients.
As salvage treatment, surgery alone was performed in 13 patients, combined treatment including surgery was performed in 12 patients, radiation or chemotherapy was performed in 13 patients, and chemotherapy alone was performed in 8 patients. The remaining 10 patients did not receive any treatment, 5 of whom died during the study period, while the remaining of 5 patients survived with recurred disease. A total of 15 patients died due to the of recurred disease, and the 5-year survival rate of patients with recurrent OPSCC was 43.9% (Fig. 1).
Prognostic factors associated with the survival of recurred patients were assessed using multivariate analysis. The predictors of successful salvage treatment were adjuvant therapy and p16 status (Table 2). Among patients with recurrent OPSCC, p16-positive patients had a 5-year disease-specific survival rate of 64% following salvage treatment and p16-negative patients showed a 5-year disease-specific survival of 30% (Fig. 2). The 5-year survival rate of patients who underwent salvage treatment including surgery was 56%, and the 5-year survival rate of patients who underwent non-surgical salvage treatment was 34% (Fig. 2). The 5-year survival rate of patients who received adjuvant therapy was 22%, and the 5-year survival rate of patients who did not received adjuvant therapy was 64% (Fig. 2).
The 5-year survival rate of patients with single lymph node recurrence was 57.2%, and the 5-year survival rate of the remaining OPSCC patients with other recurrence patterns was 40.4%, showing no statistically significant difference (Fig. 3). The 5-year survival rate of patients with local recurrence was 38%, that for patients with regional metastasis was 47%. No significant difference was observed between these two groups (Fig. 3). Clinical information of patients who expired after salvage therapy is in Supplementary Table 1.
DiscussionIn this study, the 5-year disease-specific survival of OPSCC patients who recurred after transoral surgery with/without adjuvant therapy was 43.9%. The possibility of performing salvage surgery in patients with recurrent head and neck cancer is a major prognostic factor associated with successful salvage treatment. Among the 57 recurrent patients included in this study, only salvage surgery was performed in 13 cases, combination therapy including surgery was performed in 12 cases, radiation or chemotherapy was performed in 13 cases, and chemotherapy only in 8 cases. The 5-year survival rate of patients who received salvage treatment including surgery was 64%, and that for the remaining patients was 30%. Although the patient group who underwent salvage surgery had a higher 5-year survival rate, no significant difference was found between the two groups. In OPSCC patients who recurred after transoral surgery, HPV status was a predictor of successful salvage treatment. In recurrent cancer, HPV-positive OPSCC showed better treatment results than HPV-negative OPSCC. Although the loco-regional recurrence rate is high in patients with HPV-positive OPSCC who do not receive adjuvant therapy after surgery, survival was not inferior if appropriate salvage treatment was performed [8,9]. This is presumed to be due to the biological characteristics of HPV-positive OPSCC and its high sensitivity to radiation therapy even in recurrent cases.
When recurrence patterns were analyzed, regional recurrence was most common, accounting for 58% of the total. Local metastases were present in 14% of cases, and the remaining patients showed loco-regional recurrence. Previous studies on patients with recurrent head and neck cancer reported that those with isolated neck recurrence (N1) were ideal candidates for salvage treatment [10]. Among patients with recurrent OPSCC in this study, the 5-year survival rate of 30 patients with isolated nodal recurrence was numerically higher than the rest of the patients, but the difference was not significant between the two groups. In addition, to analyze the survival rate of patients according to recurrence pattern, the 5-year survival rates of patients with local metastasis and of patients with regional recurrence were compared and analyzed, but no significant difference was observed.
The reasons why upfront surgery is preferred for treatment of OPSCC are as follows. Accurate tumor stage calculation is possible through analysis of surgical samples, and pathological factors including surgical margin, LVI, PNI, and ENE can be analyzed to determine whether to implement adjuvant therapy. We analyzed whether margin status, LVI, PNI, and ENE findings at the time of the first operation were associated with the success rate of salvage treatment in OPSCC patients. However, in multivariate analysis, these pathologic findings did not show a significant association with the survival of recurrent OPSCC patients. Since adjuvant treatment was frequently administered to groups with high levels of ENE and LVI, the prognosis for these groups was poor. Previous studies have reported poor prognosis when loco-regional recurrence occurred in patients who underwent surgery and adjuvant therapy at the time of initial treatment. This is because, in local recurrence in the area of radiation therapy or surgery, radiation therapy cannot be repeated, and further resection is often difficult [9]. These results are consistent with the results obtained in this study.
In conclusion, in OPSCC patients who recurred after transoral surgery with/without adjuvant therapy, the salvage treatment success rate was 43.9%. In recurrent cancer, HPV status was an important factor associated with successful salvage treatment, and the success rate of salvage treatment was remarkably high in patients who did not receive adjuvant therapy initially. Therefore, it is important to perform an initial surgery with a clear margin and to establish an optimal indication for adjuvant therapy.
Supplementary materialsThe Supplement is available with this article at https://doi.org/10.3342/kjorl-hns.2024.00304.
Supplementary Table 1.Clinical information of patients who expired after salvage therapy (n=21) enrolled in the study ACKNOWLEDGMENTSThis work was supported by a National Research Foundation of Korea (NRF) grant funded by the Korean government (MSIT) (NRF-2020R1F1A1052903).
NotesAuthor Contribution Conceptualization: Yoon Woo Koh, Se-Heon Kim, Jae-Yol Lim. Data curation: Dae Hyeon Kim, Yoon Woo Koh, Se-Heon Kim, Jae-Yol Lim. Methodology: Yoon Woo Koh, Se-Heon Kim, Jae-Yol Lim. Resources: Yoon Woo Koh, Jae-Yol Lim. Supervision: Yoon Woo Koh, Se-Heon Kim, Jae-Yol Lim. WritingвАФoriginal draft: Moon su Kwak, Young Min Park. WritingвАФreview & editing: Dae Hyeon Kim. Fig.¬†2.The 5-year survival rate of patients with oropharyngeal cancer according to various factor. A: Among patients with recurrent oropharyngeal squamous cell carcinoma, p16-positive patients had a 5-year disease-specific survival rate of 64% following salvage treatment and p16-negative patients showed a 5-year disease-specific survival of 30%. B: The 5-year survival rate of patients who underwent salvage treatment including surgery was 56%, and the 5-year survival rate of patients who underwent non-surgical salvage treatment was 34%. 
Fig. 3.The 5-year survival rate of patients with oropharyngeal cancer according to recurrence patterns. A: The 5-year survival rate of patients with single lymph node (LN) recurrence was 57.2%, and the 5-year survival rate of the remaining oropharyngeal squamous cell carcinoma patients with other recurrence patterns was 40.4%, showing no statistically significant difference. B: The 5-year survival rate of patients with local recurrence was 38%, that for patients with regional metastasis was 47%. No significant difference was observed between these two groups. 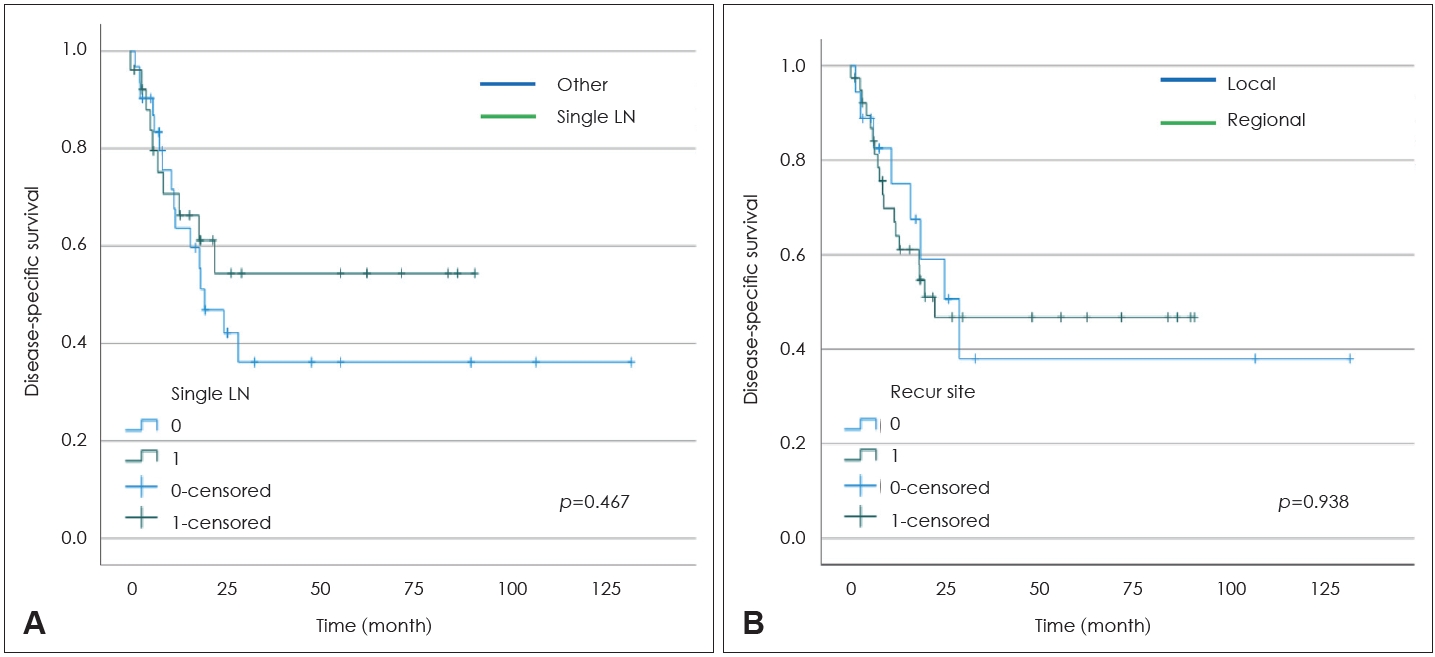
Table¬†1.Clinical information of all patients enrolled in the study (n=57) Table¬†2.Multivariate Cox regression analysis for disease-specific survival on various factors REFERENCES1. Ellington TD, Henley SJ, Senkomago V, OвАЩNeil ME, Wilson RJ, Singh S, et al. Trends in incidence of cancers of the oral cavity and pharynxвАФUnited States 2007вАУ2016. MMWR Morb Mortal Wkly Rep 2020;69(15):433-8.
2. Lim GC, Holsinger FC, Li RJ. Transoral endoscopic head and neck surgery: the contemporary treatment of head and neck cancer. Hematol Oncol Clin North Am 2015;29(6):1075-92.
3. Parsons JT, Mendenhall WM, Stringer SP, Amdur RJ, Hinerman RW, Villaret DB, et al. Squamous cell carcinoma of the oropharynx: surgery, radiation therapy, or both. Cancer 2002;94(11):2967-80.
4. Bollig CA, Morris B, Stubbs VC. Transoral robotic surgery with neck dissection versus nonsurgical treatment in stage I and II human papillomavirus-negative oropharyngeal cancer. Head Neck 2022;44(7):1545-53.
5. Park YM, Lee JG, Lee WS, Choi EC, Chung SM, Kim SH. Feasibility of transoral lateral oropharyngectomy using a robotic surgical system for tonsillar cancer. Oral Oncol 2009;45(8):e62-6.
6. Park YM, Kim HR, Cho BC, Keum KC, Cho NH, Kim SH. Transoral robotic surgery-based therapy in patients with stage III-IV oropharyngeal squamous cell carcinoma. Oral Oncol 2017;75:16-21.
7. Park YM, Kim WS, Byeon HK, Lee SY, Kim SH. Oncological and functional outcomes of transoral robotic surgery for oropharyngeal cancer. Br J Oral Maxillofac Surg 2013;51(5):408-12.
8. Carey RM, Shimunov D, Weinstein GS, Cannady SB, Lukens JN, Lin A, et al. Increased rate of recurrence and high rate of salvage in patients with human papillomavirus-associated oropharyngeal squamous cell carcinoma with adverse features treated with primary surgery without recommended adjuvant therapy. Head Neck 2021;43(4):1128-41.
|
|
|||||||||||||||||||||||||||||||||||||||

 |
 |