Introduction
Foreign bodies (metallic or non-metallic) in the upper airway are relatively commonly encountered in the emergency department or outpatient clinic. In most instances, they can be easily located and removed by means of direct laryngoscopy. However, sharp foreign bodies may occasionally penetrate soft tissue and become difficult to locate. If not removed, a foreign body can cause serious complications such as deep neck infection and/or mediastinitis; surgical removal through transcervical exploration is required.
We encountered a patient with a psychiatric disorder who had ingested multiple sewing needles. The needles deeply penetrated into soft tissue around the vocal cords, requiring removal with the aid of intraoperative C-arm fluoroscopy. Herein, we describe this successful retrieval and review the relevant literature.
Case
A 30-year-old female with type 2 bipolar disorder visited the emergency room with a sore throat and dysphagia. The patientŌĆÖs mother reported that the patient had swallowed approximately 10 sewing needles, 5 days prior. The patient did not complain of dyspnea and exhibited no signs (wheezing or stridor) of acute airway obstruction.
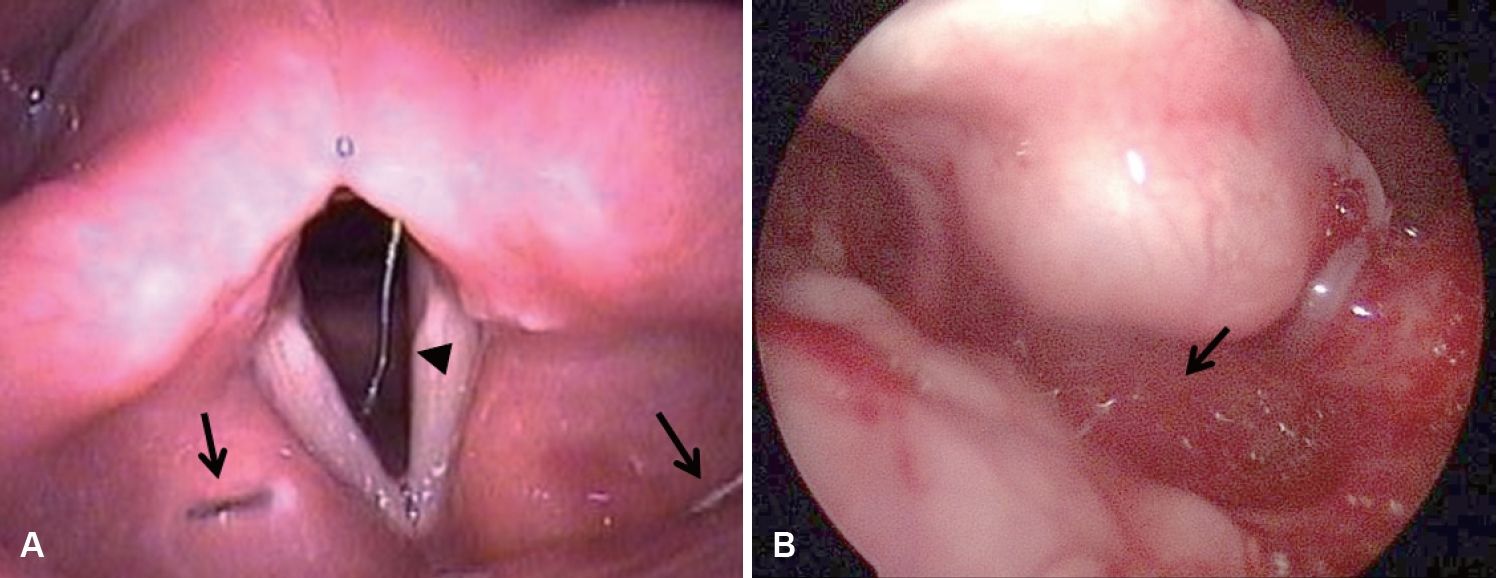
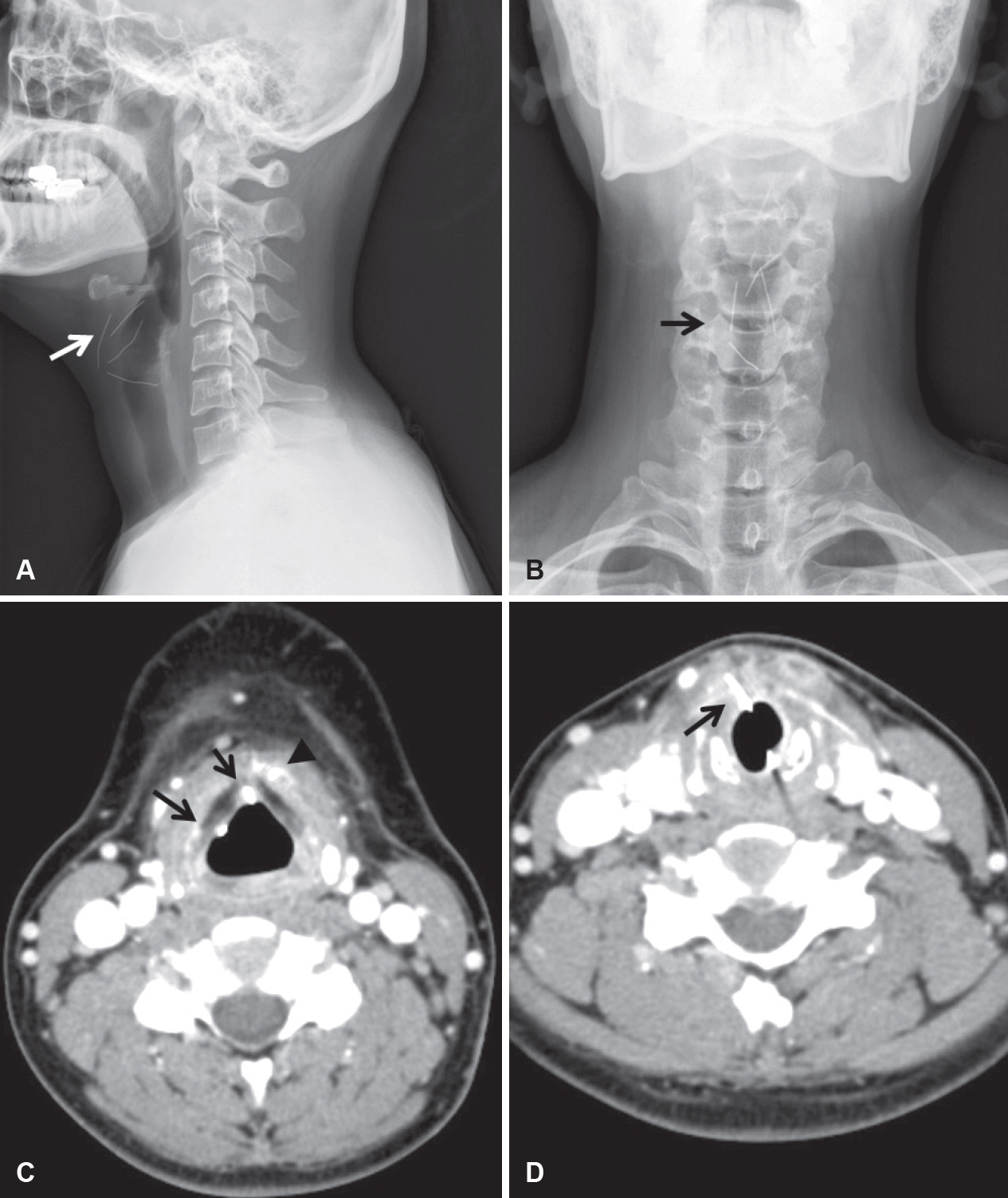
Flexible laryngoscopy revealed a single needle lodged in the subglottis and crossing the airway (Fig. 1A). Two additional needles were found in the false vocal cords on 70┬░ direct laryngoscopic examination. Mucosal swelling of the valleculae and epiglottis was evident (Fig. 1B). Simple X-rays and computed tomography (CT) scans of the neck and abdomen were acquired (Fig. 2). On the neck anteroposterior and lateral views, four metallic objects were evident: three in the supraglottis and one at the subglottic level. Abdominal imaging revealed eight needles in the stomach and small intestine.
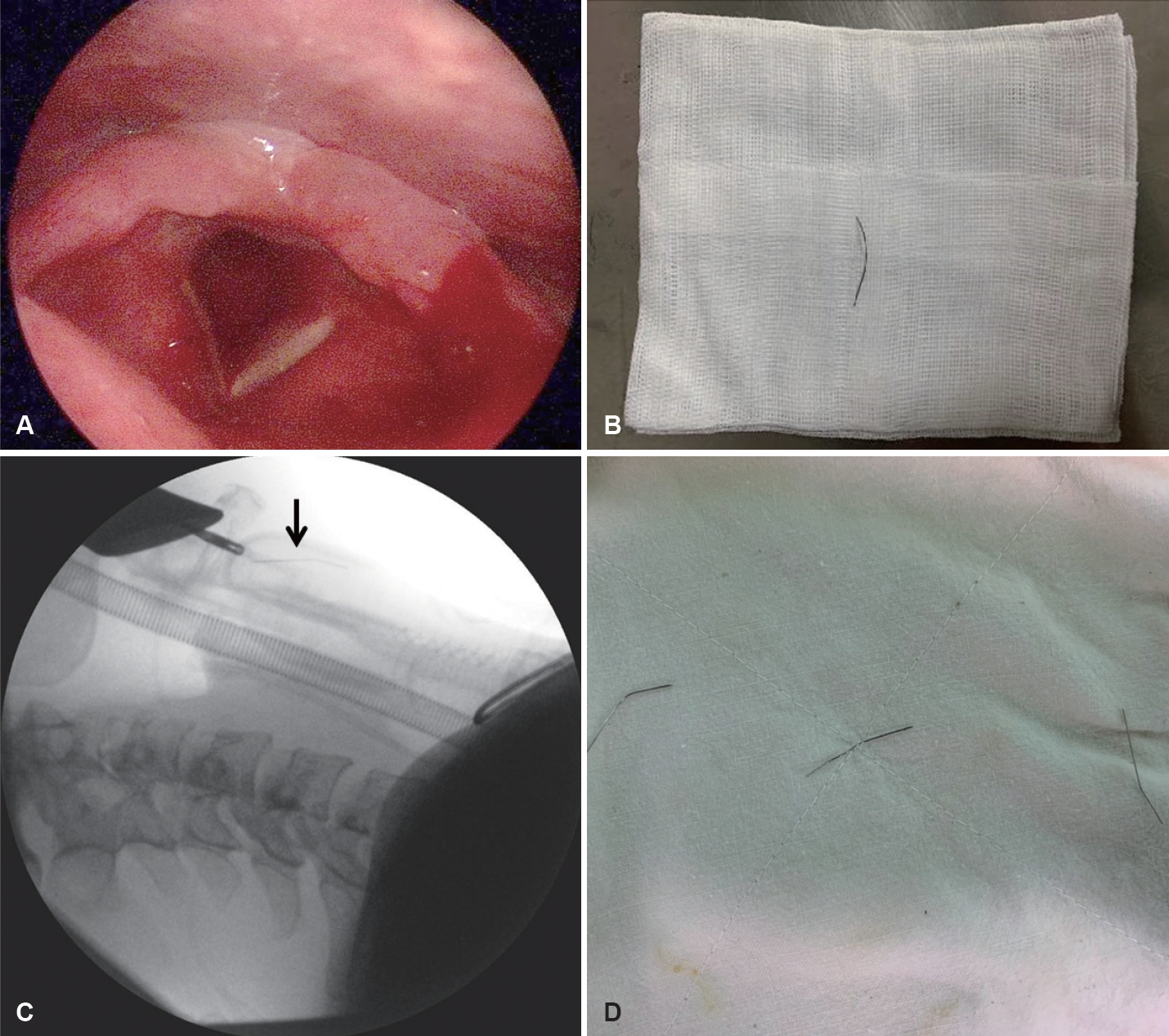
Flexible laryngoscopy was repeated to identify one needle that had not been detected previously; however, this failed because of swelling and inflammation of the vallecular area. We assumed that the needle might have penetrated deeply; thus, we decided to search for it under general anesthesia. Before intubation, we had to remove the needle lodged in the subglottis due to a risk of being pushed down to the trachea. We applied 0.1 g/mL lidocaine solution by spraying the solution five times on ventral surface of tongue, soft palate, posterior wall of oropharynx and larynx. 10 minutes after topical anesthesia, the patient was asked for the so-called ŌĆśsniffingŌĆÖ position (head extended on the neck, neck flexed on the body) while sitting on the ENT chair. The needle lodged in the subglottis was successfully removed using 70┬░ direct laryngoscopy and the curved laryngeal cup forceps (Fig. 3A and B).
Following removal of that needle, two additional needles in false vocal cord were retrieved under general anesthesia. Another one needle which was noticed at vallecular fossa in CT scan could not be found, despite the aid of suspension laryngoscopy. Because sewing needles are radiopaque, intraoperative C-arm fluoroscopy was used to locate the missing needle (Fig. 3C). As we suspected, it was deeply embedded in the vallecular area. Because the mucosal swelling of the epiglottis and valleculae was severe, the needle was retrieved via mucosal incision and dissection after its exact position had been defined (Fig. 3D).
The next day, three needles in the pylorus and duodenum were removed via esophagogastroduodenoscopy. The patient was transferred to the department of general surgery for removal of the six remaining needles (in the gastrointestinal tract) via open laparotomy under general anesthesia. However, the patient refused surgical treatment, discharged herself, and was then lost to follow-up.
Discussion
Foreign bodies lodged in the throat are commonly encountered (usually in children) in otolaryngology clinics. Foreign body ingestion in adults is often associated with mental retardation, alcohol consumption, or a psychiatric disorder [1]. Long-term embedded foreign bodies may cause vocal cord paralysis, esophageal perforation, deep neck abscess, or mediastinitis [2]. Foreign bodies must be removed immediately.
In the past, gross examination via direct laryngoscopy was routinely performed in patients with pharyngeal or laryngeal foreign bodies. Using this method, the visual field is narrow and the diagnostic accuracy is inadequate, especially with respect to very small foreign bodies [3]. Moreover, laryngoscopy is not particularly useful for detection of soft tissue-embedded materials; soft tissue retraction and mobility during examination renders foreign body localization difficult. Thus, conventional radiological and CT imaging should be routinely used to locate such objects. Magnetic resonance imaging (MRI) and ultrasound may be useful alternative methods.
The imaging modality should be chosen with reference to foreign body position, composition, and size [4]. Plain X-rays were preferred in the past; these detect most foreign bodies in a rapid and inexpensive manner, in combination with relatively low radiation exposure. Metal, glass, and gravel are radiopaque; multi-view X-ray imaging is very sensitive and specific. However, it can be difficult to detect radiolucent objects comprising wood or plastic, as well as organics such as thorns or spines; their densities are similar to the density of soft tissue. CT is more suitable for distinguishing items that differ slightly in terms of density; it reveals inflammation, abscesses, and granulomas, while providing three-dimensional data. CT-mediated detection of all types of foreign bodies has been associated with a sensitivity of 68% and a specificity of 87% [5]. MRI is most sensitive for detection of organic material. Pattamapaspong, et al. [6] found that MRI exhibited good sensitivity and specificity in terms of detecting various types of foreign bodies in the forefoot. However, MRI does not effectively detect gravel or metallic foreign bodies, as ferromagnetic artifacts develop. Ultrasound can also be used to detect foreign bodies that are deeply embedded in the throat; it involves no radiation exposure, allows real-time imaging, and is relatively inexpensive. Moreover, endoscopic ultrasound can be used during esophagogastroduodenoscopy [7]. The sensitivity of ultrasound detection is generally similar to that of CT, but better if the foreign body exhibits low radiopacity [8]. However, ultrasound probes are not suitable for deep narrow spaces, such as the hypopharynx and larynx.
Generally, most foreign bodies can be easily removed via direct endoscopy in the outpatient clinic. However, it can be challenging to locate deeply embedded, sharp foreign bodies that cannot be visually identified. Surgical exploration through transcervical approach can be considered in case of foreign bodies that cannot be detected via laryngoscopy. Therefore removing submucosal foreign bodies via small mucosal incision using radiographic modality is meaningful in that invasive surgical procedures including skin incision can be avoided. C-arm fluoroscopy is very simple and is useful for detection of metallic foreign bodies. The technique is commonly used in ophthalmology, gastroenterology, and emergency departments [9-11]. In the past, metal detectors were widely employed to detect ingested, metallic foreign bodies (e.g., coins), but such detectors are difficult to use in the operating room [12]. C-arm fluoroscopy yields real-time three-dimensional images. Cohen, et al. [11] found that the technique was suitable for detection of gravel, glass, and metal, but not wood or plastic. Immediate viewing at various angles allows the operator to perform stereotaxic navigation, reducing the operation time. The images are very valuable, but the relatively low-level radiation exposure (less than 0.96 ╬╝Sv/min to the surgeon) caused by the use of an image intensifier is undesirable [13] from the viewpoints of both the patient and the operating room staff.
Although the vast majority of foreign bodies can be removed endoscopically, transcervical neck exploration is occasionally necessary in cases of a deeply embedded laryngeal foreign body. For those patients, intraoperative ultrasonography can be a great help. Some authors previously discussed transcervical approach including laryngofissure and posterolateral approach in deeply embedded foreign body [14,15]. They suggested the usefulness of transcervical approach especially in patients who failed to remove foreign body endoscopically. But in current case, the needle was located far from skin more than 1 cm and it was more close to approach from visceral space, so we did not consider transcervical approach initially. In our case, we did not check ultrasonography because we already recognized the location of all the needles preoperatively by CT scan. Although intraoperative ultrasonography could be helpful for detecting deeply migrated foreign body when we plan transcervical exploration.
In conclusion, precise, preoperative, foreign body localization via physical examination and imaging; intraoperative localization with the aid of C-arm fluoroscopy; and early surgical intervention avoided the development of complications in our patient. Importantly, all needles in her throat were successfully removed.