Introduction
Vestibular neuritis (VN) is defined as a sudden unilateral loss of vestibular function [1]. It is the most common cause of acute spontaneous vertigo and the third most common cause of peripheral vestibular disease [2-4]. Since VN is mostly caused by involvement of the superior vestibular nerve, caloric test, which evaluates the unilateral vestibular deficit by studying the vestibulo-ocular reflex (VOR) of the horizontal semicircular canal, has been widely used as a gold standard for VN diagnosis. This examination allows quantitative evaluation of vestibular function by comparison of the results to those of the contralateral side. However, caloric test stimulates non-physiologic low VOR frequencies (0.002-0.004 Hz), and normal results can be obtained in some cases of VN involving the inferior vestibular nerve.
Recently, a new quantitative test of vestibular function, known as the video head impulse test (vHIT), has been developed. vHIT is known to have better sensitivity and specificity than the bedside head impulse test [5]. It also stimulates more physiologic high frequencies (2-5 Hz) compared to the caloric test [6]. The sensitivity of the vHIT largely correlates with that of the caloric test in the acute phase of peripheral vestibulopathy. However, several studies have reported dissociation in the results between these two tests in the nonacute phase of VN [7-9]. Most of these reports were based on comparisons of results at the time of the test. To compare these two tests more thoroughly, investigating the results longitudinally is necessary. Although a few studies have reported results of longitudinal comparison, their follow-up period was relatively short (within 3 months) [7,8]. Considering that the remaining canal paresis (CP) obtained from the caloric test is approximately 30% after one year of onset of the condition [10], it is more reasonable to evaluate the results with a longer follow-up period. Therefore, the objective of this study was to compare caloric test and vHIT results after more than 6 months of follow-up and analyze changes in their results in patients with unilateral VN.
Subjects and Method
Patients
Between September 2013 and December 2015, 48 patients were initially diagnosed with VN through caloric test. Of these 48 patients, charts from the thirteen patients who underwent an additional caloric test or vHIT at follow-up were retrospectively reviewed (Table 1). The included patients consisted of eight men and five women who ranged in age from 29 to 82 (mean: 54.3±14.3) years. Caloric tests were conducted in nine patients, and vHITs were conducted in ten patients. To thoroughly compare the changes in the results of the two tests, data from the six patients who underwent both tests were analyzed separately. All enrolled patients underwent vHITs or caloric tests within one month after experiencing symptoms of dizziness. In cases where patients received both tests during follow-up, the vHIT and caloric tests were performed on the same day. The mean follow-up duration was 13.8±11.9 months (range: 6-50 months). The Local Ethical Committee of Yonsei University approved this study (approval number: 4-2015-0534).
Caloric tests and vHITs
Detailed processes of the caloric tests and vHITs were described in our previous study [11]. A conventional bi-thermal caloric test was performed with a binocular video oculography system (SLMed, Seoul, Korea) with the patient in a supine position with 30° of head flexion. Each ear canal was stimulated for 30 seconds separately with water at temperatures of 30°C and 44°C, with a pause of 5 minutes between the two. CP in the caloric response was quantified according to Jongkee’s formula [12]. A CP value ≥25% was regarded as pathological according to our normative data.
We used a vHIT device (ICS Impulse, GN Otometrics, Taastrup, Denmark) to evaluate horizontal semicircular canal functions. Patients were seated upright with 30° of head flexion. A single right-handed examiner conducted head impulses by rotating the patient’s head to the right and left while the patient fixated on a stationary target on the wall at a distance of 1 meter. Head impulses were applied with a peak velocity range of 200 to 250°/s, rotation amplitude of 15-20°, and duration of 150-200 ms. A minimum of 20 horizontal head impulses were delivered randomly in the right or left direction. The software automatically calculated the gain in VOR. The vHIT was defined as pathological if the mean VOR gain was reduced below a value of 0.8 and overt and/or covert correcting saccades were recorded. In accordance with previous studies, the frequency of re-fixation saccades above -110°/s in at least 80% of impulses was considered pathological [13,14].
To compare the evolution of the caloric test with vHIT, variations of CP and vHIT gain were calculated for each patient using the following formulas: Variation of CP (ΔCP)=(followup CP-initial CP)/initial CP, Variation of gain (Δgain)=(followup gain-initial gain)/initial gain [15].
Statistical analysis
All statistical analyses were performed using SPSS software for PC, version 21 (IBM Corp., Armonk, NY, USA). Significant differences were determined using Wilcoxon signedrank tests. Additionally, linear regression analysis was performed and correlation coefficients were determined. All tests used a p-value <0.05 as the cut-off for statistical significance.
Results
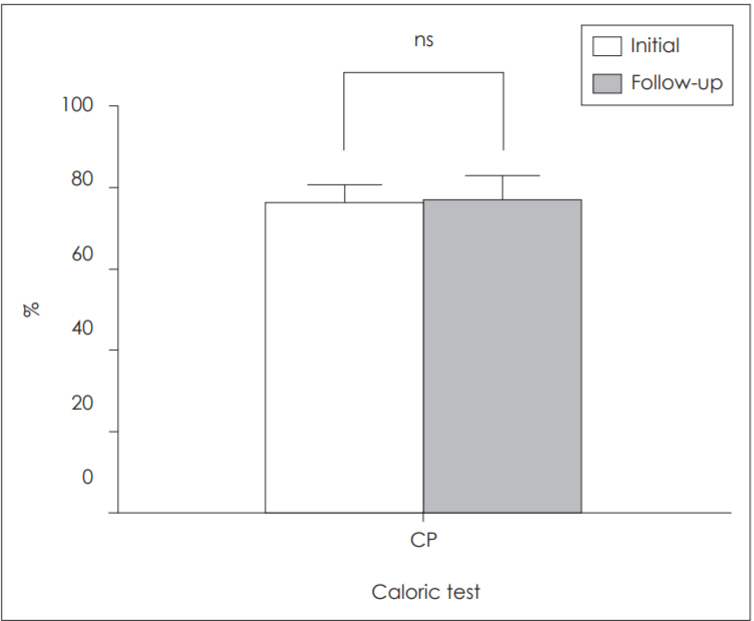
All VN patients in this study were treated with the same conventional vestibular rehabilitation protocol, which included habituation, compensation, and substitution for 1-3 months. Vestibular symptoms recovered during follow-up periods, although there were differences in recovery duration. Results of the caloric tests in the acute and chronic phases were compared in nine patients. The initial mean CP was 75.6±15.5%, and the mean CP in the follow-up test was 76.3±20.7 (Fig. 1). The mean follow-up duration was 16.9±12.4 months. There were no statistically significant differences in the mean CP between the initial and the follow-up test (p=0.889). Ten patients underwent vHIT, and their mean gains from each ear were compared. Initially, the mean gain of the affected ear was 0.58±0.21 and that of the healthy ear was 0.98±0.20. Correcting saccades were present in all patients. Among these, covert saccades were observed in seven of ten patients (70%), and overt saccades in nine patients (90%). At the follow-up test, the mean gain of the affected ear had increased significantly, to 0.79±0.21, compared to that at the initial test (p=0.011). Correcting saccades were found in five of ten patients. Of these, three patients presented covert saccades (30%) and four patients presented overt saccades (40%). The mean interval between vHIT tests was 11.7±12.4 months. The mean gain of the healthy ear did not differ significantly between the initial and follow-up tests (Fig. 2).
To determine the differences between the two tests, data from the six patients who underwent both tests were sub-analyzed. They showed no significant differences in caloric test results between the initial and follow-up tests (CP: 70.0±13.3% and 73.5±21.1% at initial and follow-up test, respectively, p=0.753). However, the vHIT showed a statistically significant improvement (mean gain: 0.56±0.24 and 0.81±0.24 at initial and follow-up test, respectively, p=0.028). Next, the correlation between variations of CP in the caloric test and horizontal gain in the vHIT was analyzed, and the improvement of horizontal gain in the vHIT was found to have no linear correlation with variations of CP (R2=0.0004, p=0.969).
Discussion
This study investigated changes in vestibular function after more than six months in patients with VN using caloric tests and vHITs. Patients with acute VN showed increased CP in the caloric test and decreased gain in the vHIT results. However, the results of follow-up showed that there were no significant changes in CP in the chronic phase, whereas the decreased gain of the vHIT showed significant recovery. The results of our study coincided with those of other studies in their results of caloric tests and vHITs. It was previously reported that 50% of patients with VN had abnormal CP after 5 or 10 years [16], and another study demonstrated that there was no correlation between CP and chronic symptoms after VN [17]. Previous studies investigating head impulses have reported that the horizontal gain increase in head impulses occurred within the first few weeks after onset [18]. Using a follow-up period of one year, Magliulo, et al. [19] have found that 85.7% of patients had resumed normal vHIT results. In addition, their multivariate regression analysis revealed that vHIT was significantly associated with clinical symptoms. However, studies assessing both caloric tests and vHIT results, and analyzing the changes between them are limited. Zellhuber, et al. [8] reported that there was no linear correlation between the gain asymmetry of vHIT and the unilateral weakness of caloric test results in a short-term 3-month analyses of individual and group studies.
In this study, six month or longer follow-up data did not show any linear correlation between changes in CP of the caloric test and horizontal gain of the vHIT. This suggests that there is no significant relationship between the degree of horizontal gain recovery and CP normalization, implying that vestibular function recovers in a frequency-specific way. Several mechanisms may explain this dissociation. First, vHITs and caloric tests have different temporal frequencies. The vHIT covers the VOR response with high frequency stimuli (2-5 Hz), which is more physiologic, while the caloric test covers non-physiological low frequency stimuli (0.002-0.004 Hz). The results of animal studies have well-established that the type of nerve fibers activated depends on the frequency of the stimuli [20]. Irregular afferents primarily encode high frequency and high acceleration head movements while regular afferents are more likely to encode low frequency and low acceleration movements [21]. Therefore, the dissociation between follow-up results of the two tests might reflect that central compensation for VOR impairment differs according to the frequency of the stimulus. Dissociation caused by different stimulus frequencies of these two types of tests has been reported in Ménière’s Disease [15].
Additionally, these two tests differ not only in their stimulated frequency, but also in their method of stimulation. While the vHIT produces a direct endolymphatic flow through head impulses, the caloric test induces an endolymphatic flow by convection heat transfer. Caloric tests also stimulate the inner ear in a gravity-independent way. Different mechanisms have been proposed such as the pressure change caused by the direct volume displacement with temperature gradient, direct thermal effect on vestibular nerve endings, and modulation of the caloric nystagmus by body position, which is produced by interaction of signals from otolith organs with those of the semicircular canal in the central vestibular nuclei [22]. These various mechanisms of stimulation could explain the remaining CP of the caloric test even after central compensation during follow up periods. Due to these differences between the two tests, the vHIT may be more physiologic than the caloric test. Furthermore, catch-up saccades were found in all patients in the acute phase. However, in the follow-up vHIT, they were observed only in some patients, and their intensity was reduced. Therefore, the vHIT may better reflect vestibular symptoms in daily life during the non-acute phase of VN. Several studies have shown that the vHIT provides information not only about vestibular impairment, but also about the effect of impairment on a patient’s quality of life [6,23]. Our results also suggest that the vHIT is more likely to be associated with vestibular symptoms than the results of the caloric test in the chronic phase of VN, since the patients’ clinical symptoms all improved but only the results of the vHIT showed significant recovery.
The present study had several limitations that prevented us from reaching more definitive conclusions. First, the number of enrolled cases in the present study was small and the follow-up period was not controlled. Additionally, there was no quantitative assessment of vestibular symptoms through indices such as the Dizziness Handicap Inventory. Further studies that consider these factors are needed. Obviously, both the vHIT and caloric tests are representative test modalities for dynamic VOR, and can provide complementary information on horizontal canal function because they stimulate different frequencies of head movement.
In conclusion, In the acute phase of VN, CP of the caloric test was increased, and the gain of the vHIT in the affected ear was decreased. Long-term follow-up showed relatively fast recovery of vHIT gain, whereas the results of the caloric test did not significantly improve. Our results suggest that the vHIT could better reflect vestibular symptoms in the nonacute phase of VN than the caloric test. However, since these two tests use different stimulus frequencies and show different recovery rates, the caloric test and the vHIT should be combined to cover a broader spectrum of frequencies and test vestibular function more precisely.