Introduction
Fungal balls are non-invasive aggregates of hyphae, primarily occurring in the maxillary sinus [1]. Most commonly composed of Aspergillus, they are often interchangeably referred to as aspergillomas [2]. These formations frequently manifest in immunocompetent patients, with occurrences documented in the middle ear or mastoid cavity [2]. While fungal balls in these regions are rare, prior cases have been reported, typically in locations readily observed during surgery [3-5]. This report presents a unique case where a fungal ball, confined to the bony portion of the Eustachian tube (ET), was encountered during endoscopic tympanoplasty. To our knowledge, this case, inclusive of intra-operative and preoperative CT images, has not been previously documented.
Case
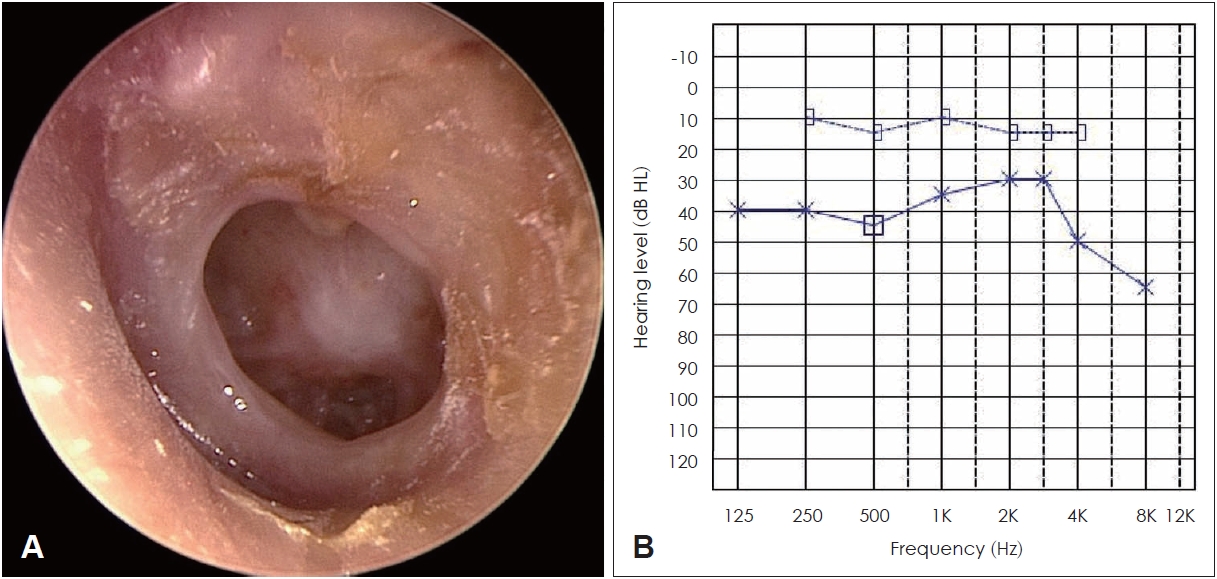
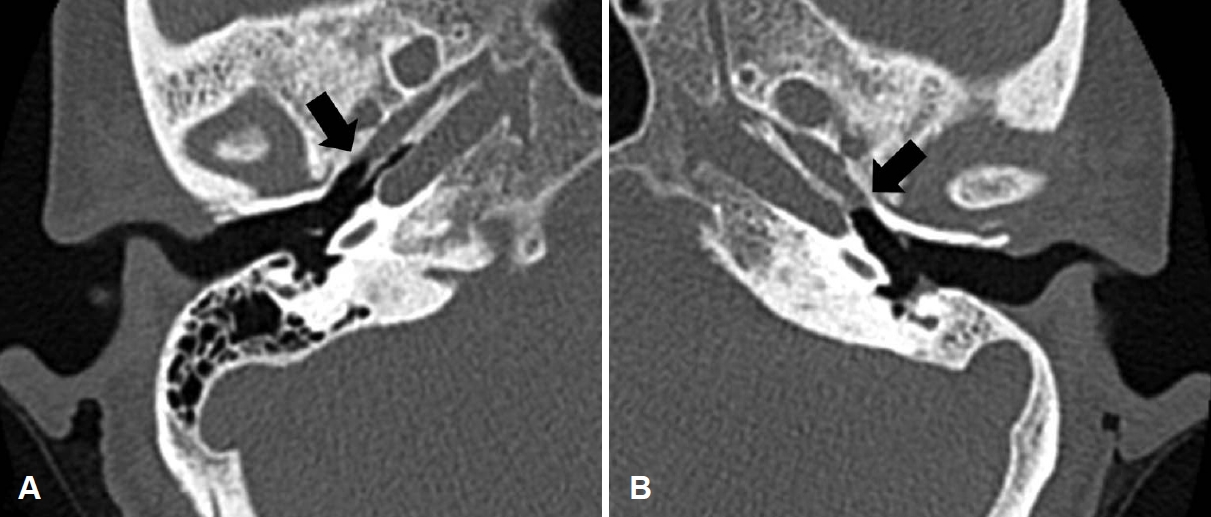
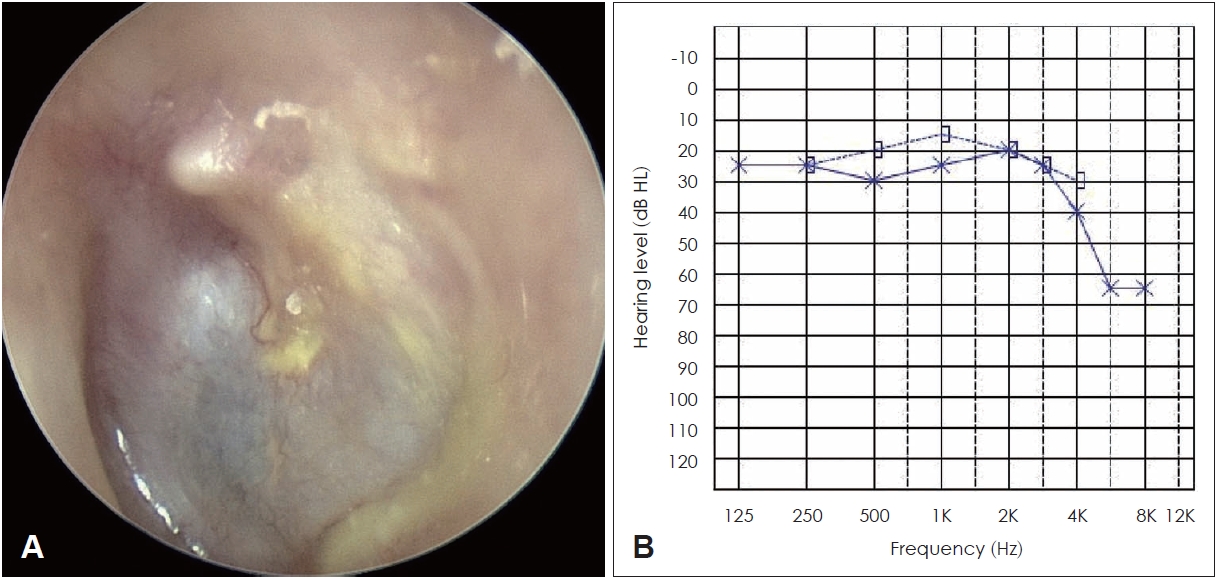
A 59-year-old female patient, without underlying diseases, presented to our clinic with a history of intermittent otorrhea persisting for approximately 20 years. The right ear exhibited normal characteristics, while the left ear displayed a medium tympanic membrane perforation with no ongoing otorrhea at the time of consultation (Fig. 1A). Pure-tone audiometry indicated a hearing threshold of 8 dB for air conduction (8 dB for bone conduction) in the right ear and 38 dB in the left ear (13 dB for bone conduction), indicative of conductive hearing loss (Fig. 1B). During an evaluation of the left ET function using the Valsalva maneuver, no sound indicative of normal tube opening was detected through the Toynbee tube. Following 1 month of confirmed absence of otorrhea recurrence, temporal bone CT imaging was conducted. The left mastoid cavity exhibited sclerotic changes, with soft-tissue density, presumed to be mucosal edema, observed in the bony portion of the ET (Fig. 2). Given the absence of otorrhea or mastoid sclerosis recurrence, endoscopic tympanoplasty without mastoidectomy was scheduled.
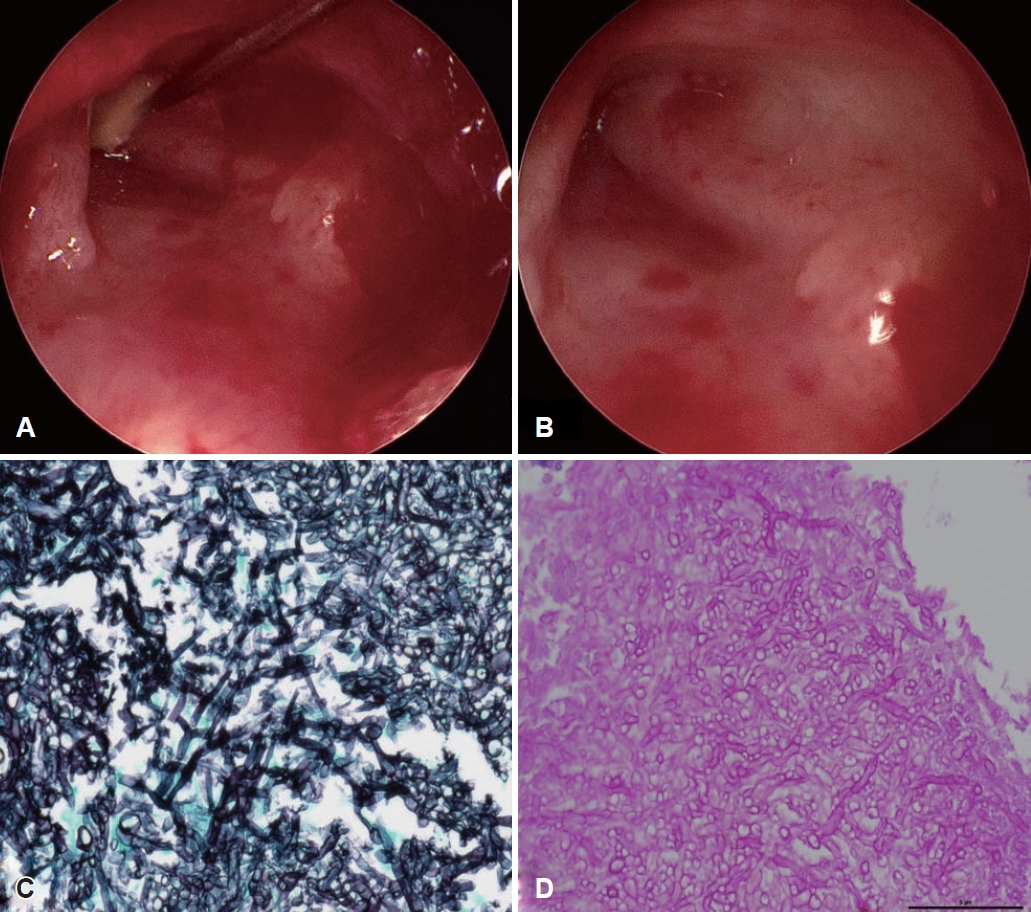
The surgical procedure entailed harvesting the perichondrium of the tragal cartilage under general anesthesia. The margin of the tympanic membrane perforation was trimmed, and the tympanomeatal flap and fibrous annulus were elevated. Due to the large size of the perforation and the observation of the bony portion of the ET, the tympanic membrane was detached from the malleus, and the ET was visualized using a 30-degree endoscope. A soft, cheese-colored mass was identified in the bony portion of the ET and subsequently removed using a pick (Fig. 3A). The mass was sent for histopathological examination, but the quantity was insufficient for additional fungal culture. Post-removal, endoscopic examination revealed erythema and edema in the mucosa of the bony portion of the ET (Fig. 3B). Following confirmation of no lesions in the middle ear, the perichondrium of the tragal cartilage was placed as an underlay above the malleus, and the middle ear was packed with Gelfoam [6]. The external auditory canal was packed with Gelfoam and rayon gauze, concluding the surgical procedure. Postoperatively, the perichondrium graft was successful, and histopathological analysis confirmed the mass from the bony part of the ET as an Aspergillus fungal ball (Fig. 3C and D). Six months post-surgery, the patientвҖҷs hearing threshold improved to 27 dB (20 dB bone conduction), and inflation of the tympanic membrane during the Valsalva maneuver became possible, indicating successful treatment with no signs of recurrence (Fig. 4).
Discussion
Fungal balls are non-invasive and typically situated extra-mucosally, causing minimal mucosal inflammation [2]. They form in the middle ear or mastoid cavity via two pathways: fungal spores either enter the middle ear through the ET after inhalation through the respiratory tract or penetrate through an already perforated tympanic membrane from the external auditory canal [1,4]. In this case, both pathways are theoretically possible. However, at the time of the patientвҖҷs visit, there were no signs of inflammation in the external auditory canal, paranasal sinuses, or respiratory tract, making it difficult to determine the exact route of entry.
Pathologically, a diagnosis of Aspergillus is established when hyphae with 45-degree angle branches are observed on gomori methenamine silver and periodic acid-Schiff stains, without invading surrounding mucosal, bony, or vascular structures [2,3]. Complete surgical removal is the preferred treatment over antifungal agents because of their non-invasive nature [2].
Fungal balls occurring commonly in the maxillary sinus typically display calcification on CT scans in approximately 80% of the cases [7]. Intralesional hyperdensity on CT indicates the presence of metal metabolites from the fungal organism [8]. In paranasal sinus fungus balls, Aspergillus, the predominant organism, utilizes its intracellular vacuole storage system to maintain zinc ion homeostasis, crucial for survival [9]. Notably, in reported cases of fungal balls in the middle ear and mastoid, calcification was not observed on CT scans [3-5]. This absence is likely due to the small size of zinc and calcium deposits, which are beyond the detection limit of conventional CT resolution [8]. While MRI could provide additional preoperative information, considering its resolution, cost, the non-invasive nature of the fungal ball, and the rarity of its localized occurrence in the ET, it may not be particularly useful [10]. Therefore, when soft tissue density is detected in the ET, it is essential to recognize that it may not signify typical mucosal edema and should be verified during surgery.
Another notable observation in this case was the localization of the fungal ball in the bony portion of the ET, a region often overlooked due to limited visibility during medial underlay tympanoplasty. To confirm the abnormal soft tissue density observed in the preoperative CT scan of the ET, the author planned lateral underlay endoscopic tympanoplasty [6]. Anatomically, as the bony portion of the ET resides in the anterosuperior quadrant, optimal visualization is achieved when a 30-degree endoscope is inserted anterior to the malleus [11]. For ET visualization, employing endoscopes with varying angles proves more advantageous than using a microscope [12]. In cases of anterior perforation, visualizing the bony portion of the ET through it is possible, but simultaneous entry of the endoscope and surgical instruments may pose challenges. Therefore, detaching the tympanic membrane from the malleus can facilitate a wider range of motion for surgical instruments.
While this case provides valuable insights into the rare occurrence of a fungal ball in the bony portion of the ET, it remains an isolated instance. More case studies or larger cohorts are necessary to understand better the pathogenesis, diagnosis, and management of fungal balls in the ET. Future studies may also explore the utility of advanced diagnostic imaging modalities, and the development of standardized surgical techniques to ensure thorough examination of this anatomically challenging region.
To our knowledge, this is the first report of a fungal ball within the bony segment of an ET. When encountering soft tissue density within the bony segment of the ET on preoperative CT, it may be misconstrued as mucosal edema; nonetheless, it is imperative not to disregard this observation. Utilizing a 30-degree endoscope can facilitate achieving a lucid view of the ET.