노인의 대사 건강과 청력 장애: 노인코호트 추적 연구
Association of Metabolic Health With Hearing Impairment Among Older Adults: A Nationwide Analysis of Follow-Up Data
Article information
Trans Abstract
Background and Objectives
To investigate the association between metabolic syndrome (MetS) and hearing impairment (HI) in elderly Korean adults using a large-scale cohort data.
Subjects and Method
Data was collected on 729664 adults who underwent at least one health screening between 2009 and 2012 from the Korea National Health Insurance Service-Senior Cohort. The study utilized a Cox proportional hazards regression model to assess the relationship between MetS and the risk of developing HI. The results were presented as an adjusted hazard ratio (aHR) with 95% confidence intervals (CI). All subjects were monitored until the occurrence of HI, death, or December 31, 2019.
Results
A total of 10102 cases of HI were identified during the follow-up period of 4920397 person-years. In the crude model, MetS was linked to an increased risk of developing HI (HR, 1.14; 95% CI, 1.10-1.19). No significant association was found after adjusting for potential confounding factors (aHR, 1.03; 95% CI, 0.99-1.08). Abnormal triglyceride (TG) levels were associated with a higher risk of HI compared to normal TG levels (aHR, 1.07; 95% CI, 1.03-1.12). In addition, the risk of HI increased as TG levels increased (>150 mg/dL).
Conclusion
Abnormalities in TG levels were independently associated with an increased risk of HI among elderly adults. Management of TG levels may protect against the risk of incident HI.
Introduction
Hearing impairment (HI) is a form of sensory deficit that is becoming an important public health issue [1]. In HI, an individual’s capacity to comprehend and use spoken language can be negatively impacted, making it more difficult for them to interact effectively with others [2]. Such communication difficulties adversely affect work productivity and cognitive or emotional status [1]. HI is a common manifestation of aging, and although it usually begins in the 30s, people typically start to experience hearing difficulties between the ages of 40 and 60 when reduced hearing ability occurs around the frequency of 1000 Hz [3]. The prevalence of HI in Korea has been reported to escalate sharply with age, from 4.4% among those aged 19-39 years to 21.1% among those aged 40-64 years and up to 69.7% among those aged 65 years or above [3]. The quality of life of individuals in their 60s is further compromised by the onset of HI, which may place a strain on the health care system [2].
Aging, loud noise, and other medical risk factors are few of the many complex physiological or pathological factors known to cause HI [3]. There is some overlap between the risk factors for metabolic syndrome (MetS) and HI [4]. One-fifth of the American population is estimated to have MetS, although this number varies widely by region and enrolled population [5]. An increasing trend of HI has been noticed in Asian countries, which poses a serious challenge to public health experts and is likely to become a social and economic problem in the near future [6]. Changes in South Korea’s social and economic environment have been among the most rapid of Asian nations, reflecting the country’s increasing westernization and the health risks associated with it. After controlling for differences in body type, the prevalence of MetS among Koreans has been reported to be higher than among whites. This is largely because of the combination of reduced physical activity and unhealthy dietary habits. Therefore, it is important to establish appropriate strategies for managing the health status of older Korean adults by understanding the impact of MetS on incident HI.
The components of MetS include insulin resistance, abdominal obesity, dyslipidemia, high blood pressure, and hyperglycemia [7]. The risks of atherosclerotic cardiovascular disease, type 2 diabetes mellitus (DM), and even death have been found to be increased by worsening of metabolic risk factors. MetS can also harm parts of the body responsible for hearing. For instance, the cochlear structure and function can be negatively impacted by dyslipidemia [4]. According to the results of a prospective study involving 1381 Korean women aged >50 years, those with MetS had a higher prevalence of high-frequency HI than those without it [8]. The number of abnormal components of MetS has been shown to be significantly associated with HI in middle-aged Koreans, but the association between MetS and older Korean adults remains unclear [9].
The current lack of consensus regarding the link between MetS and HI risk limits the recommendation of MetS as a biomarker of incident HI. Specifically, MetS was found not to be an independent risk factor for HI in Korean adults aged 19 years or above, and only fasting plasma glucose was associated with HI in the 5th Korea National Health and Nutrition Examination Survey-based cross-sectional study of 16799 participants [10]. In a cross-sectional study of 18824 middle-aged or older Chinese subjects, MetS was associated with a higher risk of hearing loss after adjustments for age, sex, smoking, alcohol consumption, family history of deafness, ototoxic drugs, history of occupational noise exposure, lipid and blood pressure lowering drugs, and antidiabetic medications [11]. However, a nationwide cohort study of 11457931 Korean adults aged at least 40 found a negative association between MetS and hearing loss after adjustments for age, sex, smoking, alcohol habitus, exercise, income, body mass index, and ear disease [12]. Considering that the association between MetS and HI is yet controversial, and related evidence in literature is especially poor in older adults, the purpose of this study was to investigate the association between MetS and HI in elderly Korean individuals.
Subjects and Methods
Study population
The study sample was drawn from individuals who were enrolled in the National Health Insurance Service (NHIS) of Korea, which offers compulsory healthcare insurance services to up to 97% of the Korean population. The NHIS collects data on health screening results, hospitalization and visits, medical treatment, and pharmaceutical prescriptions. The NHIS provides biennial health screening for all employed and insured participants. The NHIS-Senior cohort v2.0 is a hybrid cohort that combines both prospective and retrospective data collection methods. It is a nationwide study that included 511953 adults aged 60 years or older in 2008. The participants were selected randomly from a total of 6.4 million older adults. Data on individuals who were 60 years old after 2008 were also collected. Information was collected retrospectively and prospectively from 2002-2007 and after 2008, respectively.
Data on a total of 756933 older adults who had at least one health screening examination between 2009 and 2012 were obtained from the NHIS-Senior database, including the NHIS-Senior cohort v2.0. Those with death (n=11470) or HI (n=10155) prior to the follow-up investigation were excluded. Furthermore, participants with missing information on metabolic risk factors (n=533) and missing information for other key variables (n=5111) were excluded. The final analytical cohort included 729664 older adults (Fig. 1). The study followed all subjects from the date of their health screening examination until December 31, 2019, or until the occurrence of an event, whichever came first.
Ethical consideration
This study complies with the Declaration of Helsinki and was performed according to ethics committee approval (JEJUNUH 2021-09-007). The NHIS database was made available to the researchers under strict confidentiality guidelines and after anonymization; therefore, the requirement for informed consent was waived.
MetS
The study used the National Cholesterol Education Program-Adult Treatment Panel III guidelines, which were modified for Asian populations, to define MetS [8]. The participants were diagnosed with MetS if they had at least three of the following five conditions: 1) waist circumference ≥90 cm (men) or ≥80 cm (women), 2) triglyceride (TG) levels ≥150 mg/dL, 3) high-density lipoprotein cholesterol (HDL-C) levels <40 mg/dL (men) or <50 mg/dL (women), 4) blood pressure ≥130/85 mm Hg or prescription of antihypertensive medications, and 5) fasting serum glucose levels ≥100 mg/dL or prescription of antidiabetic medications.
HI
Hearing impaired was defined and registered according to the Korea Presidential Decree No. 32364 Enforcement Decree of the Welfare Act for the Disabled criteria, which included hearing loss of at least 60 dB for both ears or hearing loss of at least 80 dB for one ear and at least 40 dB for another ear after three evaluations using a pure tone audiometry test (PTA) and one evaluation using an auditory brainstem response. The average PTA hearing threshold was calculated as follows: (500 Hz + 2×1000 Hz + 2×2000 Hz + 4000 Hz)/6.
Key variables
Blood pressure was measured using sphygmomanometer or oscillometric device after a rest of 3 to 5 minutes. A staff chose an appropriate-size cuff, and repeated the measurements for at least 2 times at an interval of 1 to 2 minutes. The baseline blood pressure was defined as the mean value of blood pressure. Trained examiners measured the middle of the rib cage and iliac crest in centimeters for the measurement of waist circumference. For the adjusted analysis, we included the following variables: household income (categorical; upper and lower half), age (continuous; years), sex, body mass index (continuous; kg/m2), DM (categorical; yes and no), hypertension (categorical; yes and no), dyslipidemia (categorical; yes and no), moderate-to-vigorous physical activity (MVPA; categorical; 0, 1-2, 3-4, and ≥5 times/week), smoking (categorical: never, former, and current), alcohol consumption (categorical; yes or no), and Charlson comorbidity index (CCI; categorical; 0, 1-2, and ≥3). Household income was determined using the insurance premiums, which serves as a proxy for income status in the NHIS database [13]. We used the 10th International Classification of Diseases codes for DM (E10-E14), hypertension (I10), and dyslipidemia (E78), along with prescriptions of antidiabetic, antihypertensive, and antidyslipidemic drugs to define DM, hypertension, and dyslipidemia, respectively. The study calculated the CCI using the 10th Revision of the International Classification of Diseases [14].
Statistical analysis
The study used a Cox proportional hazards regression model to evaluate the risk of developing HI, and the hazard ratios (HRs) and 95% confidence intervals (CIs) were calculated. To illustrate the relationship between TG levels and the incidence of HI, a restricted cubic spline was plotted with three knots located at the 5th, 50th, and 95th percentiles. Sensitivity analyses were also performed to exclude cases of developing HI prior to the follow-up investigation by removing participants who had experienced HI events within 1, 2, 3, 4, and 5 years from the initial follow-up date. The study performed subgroup analyses by stratifying the participants by age, sex, obesity, hypertension, DM, dyslipidemia, and MVPA.
The study assessed the correlation between MetS and the risk of HI using three models: 1) non-adjusted (crude model), 2) adjusted for age and sex, and 3) adjusted for age, sex, household income, body mass index, hypertension, DM, dyslipidemia, smoking, alcohol consumption, MVPA, and CCI.
The main analysis was based on the final model, which was adjusted for all potential confounding factors. A two-sided p-value of less than 0.05 was considered statistically significant. The data collection, mining, and analyses were conducted using SAS Version 9.4 (SAS Institute, Cary, NC, USA) and R Version 3.3.3 (R Foundation for Statistical Computing, Vienna, Austria).
Results
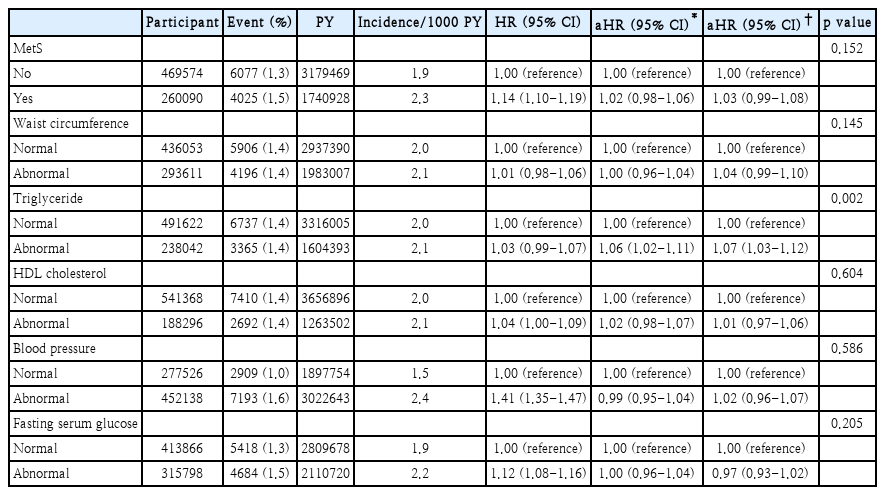
Over a period of 4920397 person-years of follow-up, 10102 cases of incident HI were detected. Table 1 provides an overview of the sociodemographic and descriptive features of the participants. Among 729664 participants, the median age (interquartile range) was 65 and 64 years for participants with and without MetS, respectively. In addition, the median body mass index was 25.6 and 23.2 for participants with and without MetS, respectively. Those with MetS had higher proportions of women; presented higher levels of systolic blood pressure, fasting serum glucose, and total cholesterol; were more likely to be inactive; and had hypertension, DM, dyslipidemia, and comorbidities.
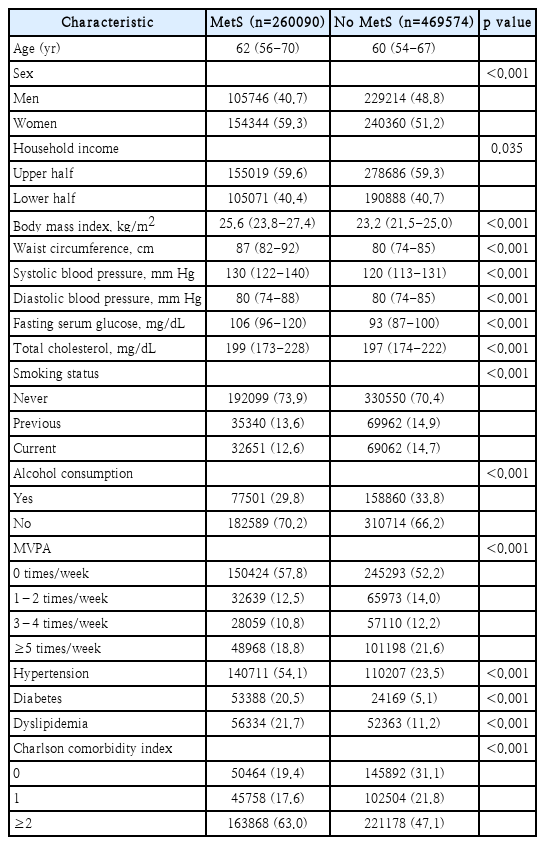
Baseline characteristics of the participants who underwent health screening according to the presence of MetS
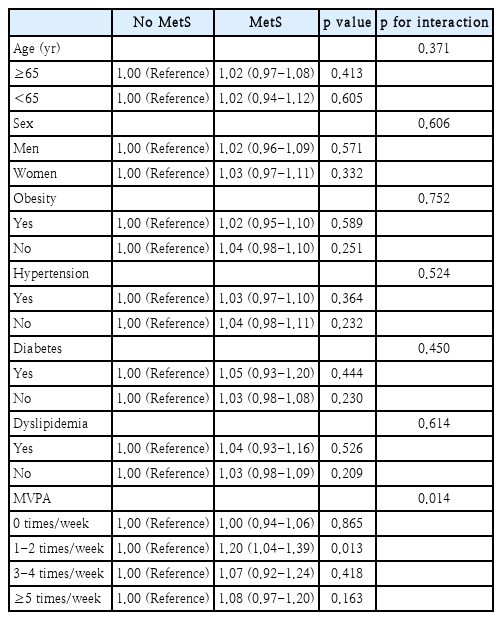
MetS was linked to an increased risk of incident HI (HR, 1.14; 95% CI, 1.10-1.19) in the crude model, as shown in Table 2. However, no significant association was observed after adjustment. In addition, we found no significant association between any of the MetS components and HI risk, except for TG, in the fully adjusted model. TG abnormality was associated with a 1.07-fold increased risk of HI (aHR, 1.07; 95% CI, 1.03-1.12). Fig. 2 shows that the risk of HI increased as the TG levels increased (>150 mg/dL).
Restricted cubic spline used for evaluating the association between TG level and risk of hearing impairment among older adults. aHR calculated after adjustments for age, sex, household income, body mass index, hypertension, diabetes, dyslipidemia, smoking, alcohol consumption, moderate-to-vigorous physical activity, and Charlson comorbidity index. TG, triglyceride; aHR, adjusted hazard ratio.
Table 3 displays the results of subgroup analyses that were conducted based on age, sex, obesity, hypertension, DM, dyslipidemia, and MVPA. We did not find any statistically significant interactions except for MVPA. The Supplementary Table 1 presents the results of sensitivity analyses that calculated the risk of HI after excluding events that occurred within 1, 2, 3, 4, and 5 years from the start of follow-up. The primary finding across all five washout models was that participants with MetS had a higher risk of HI than those without MetS. However, the observed difference was not statistically significant.
Discussion
In this study of Koreans aged 65 years and older, we found no evidence that MetS increased the risk of HI; however, one of its components, abnormal TG, was associated with a higher risk of incident HI. We discovered a wide range of studies, all of which reached different conclusions regarding the association between MetS and HI. Nevertheless, we could compile some evidence that elevated TG levels are associated with an increased risk of developing HI.
In a cross-sectional study of 94224 Koreans in their 40s, no association was found between MetS and HI. However, the four distinct components of MetS were found to have a significant and independent relationship with the incidence of HI after adjustments for age, sex, household income, body mass index, hypertension, diabetes, dyslipidemia, smoking, alcohol consumption, MVPA, and CCI, which were identified as risk factors for the development of HI in middle-aged or older adults [15-17].
After a one-unit increase in waist circumference, systolic blood pressure, TG, or fasting blood glucose, the participants’ risk of HI increased by 9%, 12%, 8%, and 9%, respectively [9]. Another cross-sectional study of 16799 Koreans aged above 50 years reported that MetS was not a significant predictor of HI. Among the MetS factors, only elevated fasting plasma glucose levels have been shown to be independently associated with HI [10]. A cross-sectional study conducted in the United States on 40 patients with dyslipidemia, with a mean age of 54 years, found a correlation between elevated TG levels and auditory dysfunction. This suggests that chronic dyslipidemia may impair hearing by elevating TG levels [18]. Studies on animals have shown that high levels of dietary cholesterol alone can lead to auditory impairment if hypercholesterolemia is maintained for more than a few months [19,20].
In contrast, other studies demonstrated a significant association between MetS and HI. In a cross-sectional study of 28866 Koreans with a mean age of 44 years, those with four or more MetS components exhibited a higher incidence of HI than those with fewer than two [21]. Another cross-sectional study involving 11114 Azerbaijanis confirmed that MetS was associated with a 40% increase in the risk of sensorineural HI. The risk of HI increased in proportion to the number of MetS components: 48% for MetS with four components, and 78% for MetS with five components. Nonetheless, the study discovered that each MetS component was independently associated with HI, underscoring the need to examine each MetS component in addition to itself [4]. In a cross-sectional study of 2100 adults, significant associations between the increasing number of MetS components and hearing thresholds were found. Notably, low HDL-C and high TG levels demonstrated a stronger association with HI [22]. Given the contradictory findings of previous studies, it appears that the presence of MetS is not necessarily associated with HI. The reasons for the discrepancies in HI prevalence after MetS may include differences in study size, diagnostic criteria, and genetic predispositions.
Patients with dyslipidemia have been found to experience a higher rate of sensorineural hearing loss, suggesting a link between high TG levels and HI. Elderly individuals taking hyperlipidemia medications have also shown improved hearing compared with those who do not [23]. However, the underlying biological mechanisms of TG imbalance and HI are poorly understood [24]. Evidence suggests that oxidative stress and mitochondrial DNA (mtDNA) mutations or deletions play significant roles in the development of HI [25]. Oxidative stress, which may cause irreversible hearing loss, is amplified and prolonged by lipid abnormalities [26]. An animal study have indicated that oxidative stress can cause damage to macromolecules, including mtDNA and the accumulation of mtDNA mutations or deletions and decline of mitochondrial function play an important role in inducing apoptosis of cochlear cells, which may lead to age-related hearing loss [25]. Increased oxidative stress and mitochondrial dysfunction have been observed in many organs of animals that were given a high-fat diet for a long period of time [26].
Microcirculatory disturbances associated with dyslipidemia are thought to contribute to HI. The exact mechanism by which vascular risk factors affect hearing is still unclear, but they are thought to contribute to decreased blood flow to the cochlea [27]. Sudden hearing loss, Meniere’s disease, and other inner ear disorders have all been associated with reduced blood flow to the cochlea. Hearing loss may be the result of microvascular diseases affecting the cochlear striae vascularis, such as arteriolosclerosis of blood vessels in the cochlea [28]. The production of nitric oxide (NO) can also be inhibited by dyslipidemia [9]. NO, an endothelium-derived relaxing factor, influences both vascular and neural functions. NO is produced by endothelial and smooth muscle cells in the blood vessels and aids in regulating blood flow to the cochlea. Considering NO is a vasodilator, decreased NO synthesis may lead to lower cochlear blood flow. Thus, microcirculatory disturbances and reduced NO production due to dyslipidemia may lead to hearing deterioration [29]. The vacuolar edema and vascular striatal degeneration found in guinea pigs fed a lipid-rich diet may further support this hypothesis [19]. In this research, TG level was associated with a higher risk of HI, suggesting that TG level may be an alternative indicator for the risk of HI. Taken together, dyslipidemia may contribute to an increased risk of HI in patients with MetS.
The effect of high TG levels on the risk of HI may be mediated in part by impairments in lipid metabolism, which are manifested by elevated serum TG, very low-density lipoprotein (VLDL), apolipoprotein B, and non-HDL-C levels [30]. An increase in serum TG is caused by an increase in the hepatic synthesis of VLDL particles and decrease in TG-rich lipoprotein clearance. Increases in serum TG levels are often accompanied by decreases in HDL-C. Increased TG may negatively affect HI risk because of decreased HDL-C levels because HDL-C has anti-inflammatory, antioxidant, and anti-apoptotic properties that help mitigate the pathological alterations caused by dyslipidemia [9].
Based on our research, this is one of the largest longitudinal cohort studies conducted in Korea to investigate the correlation between MetS and HI in the older population. We believe that this research will lay the groundwork for identifying potential risk factors of HI at an early stage, especially in older adults with abnormal TG levels. However, it is important to consider the following limitations when interpreting the results of this study. First, because this was a retrospective study, the association between MetS and incident HI may have been influenced by reverse causality. Second, there were insufficient data to consider the potential confounding factors, such as ototoxic drug use, noise exposure, and family history of HI or MetS, on HI [3]. In addition, the content of an individual’s diet, which has been suggested to be an important factor in causing or preventing auditory disorders [20], could not be considered. Thus, in future studies, it would be helpful to account for additional confounding factors that may further damage hearing function. Third, patients with dyslipidemia may have normal TG levels due to medication, according to our definition with diagnostic code and related medication. However, the impact of antidyslipidemic medication on HI could not be confirmed in this study, and further research is required to investigate the relationship between antidyslipidemic medication and HI. Fourth, the study only included older adults in Korea; thus, the results may not apply to other countries or ethnicities. Finally, we were unable to isolate the types of HI owing to the lack of relevant information. The NHIS-Senior cohort operationally defines HI without specifying its various types. Given that our study population had a median age of over 60 years, it is possible that the HI in this study primarily refers to sensorineural HI due to aging or other relevant causes; however, some other cases may also be included.
In conclusion, MetS was not identified as an independent risk factor for HI in Korean older adults, while TG abnormality was found to be an independent predictor of incident HI. Therefore, lowering TG levels may reduce the disease burden associated with HI. Additional research is needed to establish whether the observed associations reflect causal biological phenomena.
Supplementary Material
The Supplement is available with this article at https://doi.org/10.3342/kjorl-hns.2023.00920.
Acknowledgements
This work was supported by a grant of the Jeju National University Hospital Research Fund.
Notes
Author contributions
Conceptualization: Yun Hwan Oh, Michelle J. Suh. Project administration: Beom Sik Park. Supervision: Michelle J. Suh, Yun Hwan Oh. Validation: Hye Jun Kim, Seogsong Jeong. Visualization: Hye Jun Kim. Writing—original draft: Hye Jun Kim, Seogsong Jeong. Writing—review & editing: Michelle J. Suh, Yun Hwan Oh.